TIM-3 therapy is an innovative approach emerging at the intersection of cancer research and Alzheimer’s treatment. Recent studies indicate that inhibiting the TIM-3 molecule can enhance the brain’s immune response, specifically by enabling microglia to effectively clear amyloid plaques associated with Alzheimer’s disease. This immune checkpoint therapy, initially explored in cancer treatment, has shown promise in improving cognitive function in preclinical trials involving mice. By unlocking the capabilities of microglia, TIM-3 therapy could represent a significant advance in combating the plaque buildup that impairs memory and learning, marking a hopeful stride towards more effective Alzheimer’s interventions. As researchers continue to refine this therapy, the potential for cognitive improvement in patients could redefine our strategies against neurodegenerative diseases.
Introducing TIM-3 as a therapeutic target in neurodegenerative diseases highlights a novel use of immune checkpoint inhibitors typically reserved for oncology. By modulating the function of key immune cells, particularly those in the brain like microglia, this approach aims to address the underlying mechanisms of plaque accumulation in Alzheimer’s. Inhibitory molecules such as TIM-3 can potentially restore the natural clearance processes of the brain, offering a dual benefit of protecting cognitive functions while simultaneously tackling the neuroinflammatory aspects of Alzheimer’s pathology. This emerging strategy represents a paradigm shift in how we can leverage the body’s immune system not just in fighting cancer but also in combating Alzheimer’s disease. With ongoing research, the concept of using immune modulation for cognitive enhancement opens new avenues for therapeutic developments in the realm of Alzheimer’s treatment.
Unleashing the Power of TIM-3 Therapy for Alzheimer’s Disease
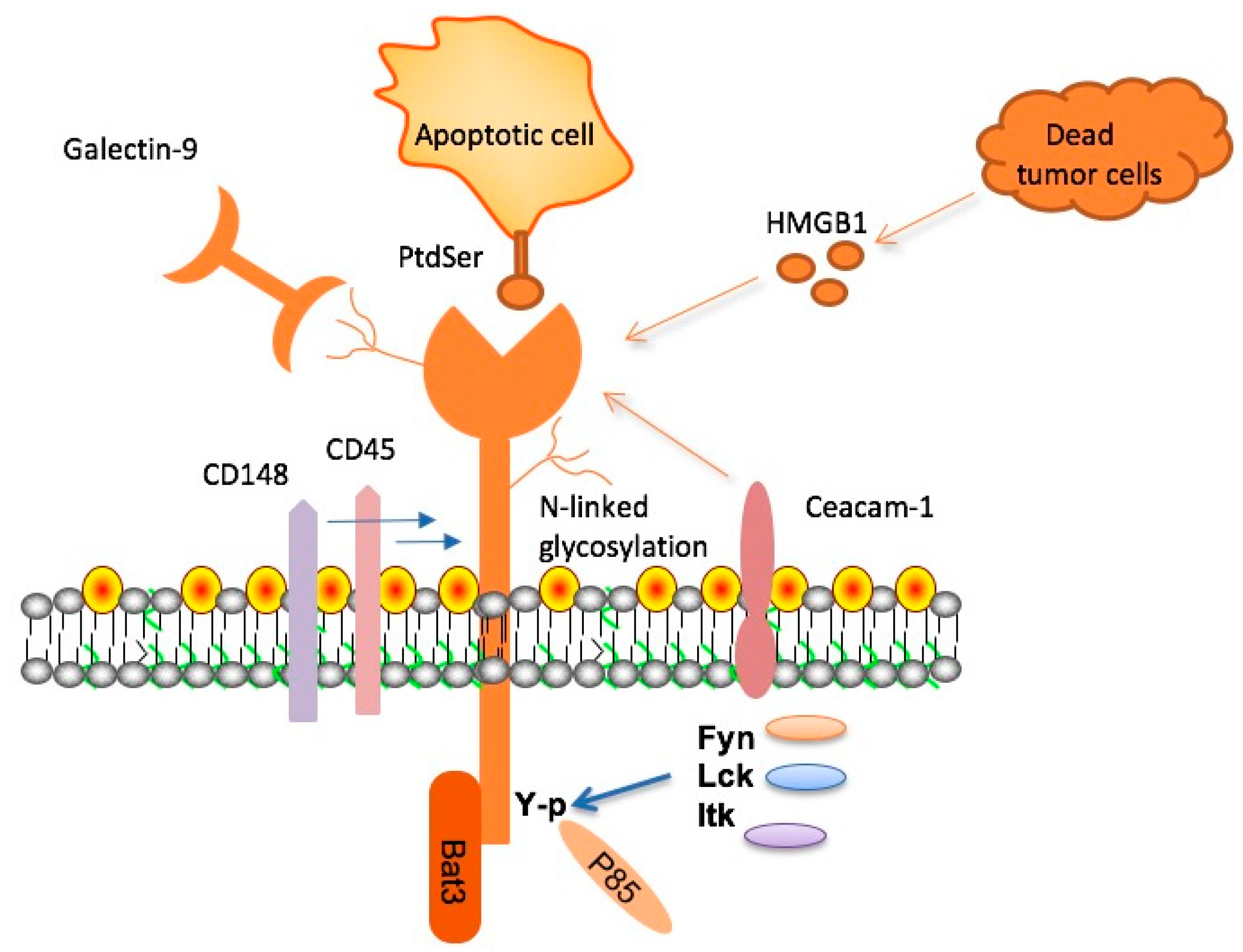
Recent advances in Alzheimer’s disease (AD) research have highlighted the significant role of TIM-3 therapy, a novel approach that might reshape the landscape of Alzheimer’s treatment. This therapy focuses on inhibiting the TIM-3 checkpoint molecule, allowing microglia— the primary immune cells of the brain— to effectively clear amyloid beta plaques. By blocking TIM-3, researchers found that microglia could regain their ability to combat these pathological structures, which are hallmarks of Alzheimer’s. This paradigm shift suggests that mechanisms used successfully in cancer treatment could be repurposed to halt the progressive cognitive decline associated with Alzheimer’s.
Moreover, the implications of TIM-3 therapy extend beyond mere plaque clearance. When microglia are activated and release TIM-3, they enter a homeostatic state that inhibits their plaque-fighting abilities. However, by targeting this inhibitory pathway, we may not only improve cognitive functions but also enhance the overall immune response within the central nervous system. Vanderbilt University researchers have shown that reactivating microglia through TIM-3 modulation leads to substantial cognitive improvement in animal models, raising hopes for similar advancements in human treatments.
Alzheimer’s Treatment: A Breakthrough in Immune Checkpoint Therapy
The concept of immune checkpoint therapy, traditionally applied in cancer treatment, finds promising applications in Alzheimer’s treatment. This approach harnesses the body’s immune system to unleash its full potential against Alzheimer’s plaques. Researchers, including those from Brigham and Women’s Hospital, have demonstrated that disabling checkpoint molecules like TIM-3 results in a more vigorous microglial response to damaged neurons and amyloid plaques. These insights signal a transformative shift in how we can approach Alzheimer’s, allowing for the potential of cognitive improvements that were previously unattainable.
By understanding the mechanism by which immune checkpoints function, scientists are able to tailor therapies that provoke the body’s own defenses to fight against Alzheimer’s. Existing therapies designed to inhibit TIM-3 not only promise to enhance the immune response against plaques but also hold the potential to modify the disease course. As ongoing trials continue to explore this innovative therapy, the Alzheimer’s research community is abuzz with anticipation over potential breakthroughs that could significantly improve the quality of life for millions of individuals afflicted with the disease.
Microglia and Alzheimer’s: A Symbiotic Relationship Untangled
Microglia, the brain’s resident immune cells, play a crucial role in neuroprotection and homeostasis. In Alzheimer’s disease, these cells undergo significant changes, often becoming dysfunctional in their ability to clear amyloid plaques. When microglia overexpress TIM-3, their phagocytic function is inhibited, leading to plaque accumulation. Unraveling the relationship between microglia and Alzheimer’s highlights the delicate balance between neuroinflammation and cognitive function— an imbalance that TIM-3 therapy aims to correct.
Recent findings suggest that restoring the normal functionality of microglia could greatly enhance the effectiveness of Alzheimer’s treatments. By targeting the TIM-3 molecule, researchers hope to reinvigorate these critical immune cells, allowing them to resume their tasks of clearing debris from the brain and enhancing synaptic health. This dual approach not only addresses the immediate neurodegenerative effects of Alzheimer’s but also bolsters the long-term maintenance of cognitive health, ultimately paving the way for new therapeutic avenues that promise improved treatment outcomes.
Cognitive Improvement Through Innovative Alzheimer’s Solutions
Emerging research indicates that cognitive improvement in Alzheimer’s patients may be achievable through innovative therapeutic strategies such as TIM-3 therapy. By modulating the immune response and enhancing microglial function, these new approaches have shown promising results in preclinical models. For instance, deactivating TIM-3 in murine models led to a significant decrease in plaque burden and an accompanying improvement in memory performance, suggesting a direct link between immune modulation and cognitive restoration.
In addition to potential behavioral improvements, cognitive enhancement strategies built around TIM-3 therapy offer a ray of hope for Alzheimer’s care. By focusing on the restoration of microglial activity, researchers are optimistic that future treatments could not only manage the symptoms of Alzheimer’s but also address some underlying mechanisms contributing to the disease. This shift in focus from passive management to active intervention signals a bright future for patients seeking more than symptomatic relief.
Transforming Alzheimer’s Therapy with Immune Checkpoint Modulation
The therapeutic potential of immune checkpoint modulation presents an exciting frontier in Alzheimer’s research. By employing strategies like TIM-3 therapy, researchers are launching new campaigns against the cognitive impairments associated with Alzheimer’s disease. The mechanism aims to enhance the immune capacity of microglia, thereby bolstering their ability to clear amyloid beta plaque deposits and restore brain function. This innovative approach could represent a significant leap forward in treatment efficacy.
In clinical settings, implementing TIM-3 modulation strategies could provide a multifaceted approach to Alzheimer’s therapy. The ability to harness the body’s own immune responses, similar to strategies seen in cancer therapies, holds the promise of rejuvenating neural functions affected by Alzheimer’s pathology. This unprecedented approach aligns with recent breakthroughs in cognitive research and showcases the importance of interdisciplinary studies in developing effective treatment modalities.
Examining Genetic Influences in Alzheimer’s and TIM-3 Expression
Genetic predispositions play a significant role in the manifestation of Alzheimer’s disease, with studies identifying crucial genetic variations linked to TIM-3 expression. Understanding these genetic factors offers insight into why some individuals are more susceptible to Alzheimer’s and how TIM-3 might be targeted therapeutically. Research led by teams at several renowned institutions has demonstrated that polymorphisms in the HAVCR2 gene significantly affect TIM-3 levels in microglia, influencing their ability to combat the challenges posed by amyloid plaques.
Furthermore, considering these genetic influences is essential for developing personalized medicine approaches to Alzheimer’s treatment. As genomic research progresses, the potential to tailor TIM-3 therapies to individual patients based on their genetic makeup could enhance treatment efficiency and effectiveness, opening new pathways for targeted interventions that specifically address cognitive decline stemming from Alzheimer’s.
TIM-3 and the Future of Alzheimer’s Treatment
The future of Alzheimer’s treatment is increasingly intertwined with the modulation of immune checkpoints like TIM-3. As research progresses, the application of TIM-3 therapy demonstrates potential not just in terms of clearing amyloid plaques but also in rejuvenating cognitive functions that have been compromised by the disease. This holistic approach, leveraging immune checkpoint inhibitors, positions TIM-3 at the forefront of new therapeutic avenues for Alzheimer’s treatment.
Continued exploration of TIM-3 modulation is critical as it aligns with advances in cancer treatment pathways. By adopting proven methodologies from oncology, Alzheimer’s research can innovate and implement strategies that address the degenerative processes affecting cognitive health. With ongoing studies now shifting towards human trials, there is renewed hope that TIM-3 therapy could offer tangible benefits for those afflicted with Alzheimer’s, potentially altering the course of future treatment paradigms.
From Cancer to Cognitive Care: A New Paradigm in Alzheimer’s Research
The leap from cancer therapies to cognitive care marks a transformative shift in how we approach Alzheimer’s disease. This cross-disciplinary synergy underlines the potential of utilizing immune checkpoint inhibitors like TIM-3 in treating neurodegenerative conditions. By effectively applying cancer-derived strategies, researchers are exploring novel ways to enhance the brain’s immune response, leading to effective plaque clearance and memory restoration in Alzheimer’s patients.
This new perspective encourages collaboration across fields, integrating oncology and neurology to tackle complex diseases like Alzheimer’s. Researchers are optimistic that successful strategies employed against cancer may one day contribute to significant cognitive improvements in Alzheimer’s therapy, transforming the therapeutic landscape and hopefully yielding groundbreaking results that enhance patients’ quality of life.
Implications of TIM-3 Research for Future Alzheimer’s Therapies
The implications of TIM-3 research extend far beyond basic science, suggesting a range of potential therapeutic applications for Alzheimer’s disease. By elucidating the cellular mechanisms that underlie immune responses and their effects on amyloid plaque clearance, researchers aim to create targeted interventions that maximize cognitive benefits. Effective TIM-3 inhibitors could serve as a cornerstone for developing treatments that not only slow down the progression of Alzheimer’s but also restore cognitive function.
Moreover, as research continues to evolve, the findings surrounding TIM-3 may influence the broader field of neurology and immunology. Insights gained from the interplay between immune checkpoints and neurodegeneration could yield additional novel therapeutic targets. As we advance, the integration of TIM-3-related research into therapeutic strategies holds great promise for unlocking new trajectories in the quest for effective Alzheimer’s treatments.
Frequently Asked Questions
What is TIM-3 therapy and how does it relate to Alzheimer’s treatment?
TIM-3 therapy is an innovative approach that utilizes the TIM-3 checkpoint molecule to enhance the immune response in the brain, specifically targeting the plaques associated with Alzheimer’s disease. By inhibiting TIM-3, researchers have found that microglia, the brain’s immune cells, can more effectively clear these plaques, potentially improving cognitive function in Alzheimer’s patients.
How does TIM-3 function in the context of Alzheimer’s disease and immune checkpoint therapy?
In the context of Alzheimer’s disease, TIM-3 acts as an inhibitory checkpoint molecule that prevents microglia from clearing amyloid plaques. By focusing on immune checkpoint therapy strategies like TIM-3 inhibition, scientists aim to unlock the potential of microglia to restore normal cognitive function by reducing plaque accumulation.
Can TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Studies involving animal models have shown that TIM-3 therapy can lead to improvements in cognitive function by enhancing the ability of microglia to clear amyloid plaques in the brain. This suggests that similar approaches in humans may offer a novel pathway for cognitive improvement in Alzheimer’s disease.
What research supports the use of TIM-3 therapy as a cancer treatment for Alzheimer’s?
Recent research highlights the effectiveness of TIM-3 inhibition, which has been successful in cancer treatments, showing promising results for Alzheimer’s. The study indicated that by deleting the TIM-3 gene in mice, the resulting cognitive improvement and plaque clearance point to a potential dual application of TIM-3 therapy in both cancer and Alzheimer’s treatment.
What role do microglia play in TIM-3 therapy for Alzheimer’s disease?
Microglia are the primary immune cells in the brain responsible for monitoring brain health and clearing harmful plaques. TIM-3 therapy aims to free these microglia from the inhibitory effects of TIM-3, enabling them to clear amyloid plaques effectively, which could lead to improved cognitive function in Alzheimer’s disease.
How is TIM-3 therapy different from traditional Alzheimer’s treatments?
Unlike traditional Alzheimer’s treatments which often focus on amyloid plaque removal without addressing immune response, TIM-3 therapy specifically targets the immune system’s regulatory mechanisms. By enhancing microglial activity through TIM-3 inhibition, it represents a novel approach to Alzheimer’s treatment that may offer more substantial cognitive benefits.
What are the future implications of TIM-3 therapy for Alzheimer’s disease?
The future implications of TIM-3 therapy for Alzheimer’s are significant. If successful in ongoing human trials, this therapy could revolutionize treatment by providing a means of reversing cognitive decline rather than simply managing symptoms. Further advancements could lead to new strategies for preventing or slowing the progression of Alzheimer’s disease.
What are the key benefits of using TIM-3 therapy for cognitive improvement in Alzheimer’s patients?
The key benefits of TIM-3 therapy for cognitive improvement in Alzheimer’s patients include enhanced plaque clearance by microglia, potential reversal of cognitive deficits, and a novel therapeutic approach that could complement existing treatments. This therapy represents hope for more effective management of Alzheimer’s disease.
| Key Points |
|---|
| Research indicates that TIM-3 therapy, an immune-system strategy, shows promise in treating Alzheimer’s disease by enhancing microglial function to clear amyloid plaques. |
| The study involved genetically modifying mice to delete the TIM-3 gene, leading to more efficient removal of plaques and improved memory functions. |
| TIM-3 is a checkpoint molecule, often inhibiting immune responses; its removal has helped restore memory and cognitive abilities in laboratory mice with Alzheimer’s. |
| Current potential treatments may involve anti-TIM-3 antibodies, which can selectively target brain plaques without affecting the vascular system. |
| The research represents a significant five-year collaboration aimed at translating findings from mouse models to potential human therapies. |
Summary
TIM-3 therapy holds the potential to revolutionize the treatment of Alzheimer’s disease by targeting the immune response to effectively clear harmful plaques from the brain. Research suggests that inhibiting the TIM-3 checkpoint molecule can enhance the ability of microglial cells to remove amyloid-beta plaques, which play a central role in Alzheimer’s pathology. As studies progress, the adaptation of TIM-3 targeted therapies offers hope amidst previous challenges in developing effective Alzheimer’s treatments.